For years, obesity has been treated like a personal failing—something that can be fixed with more willpower, a strict diet, or a punishing workout routine. But those approaches have clearly fallen short, not just for individuals, but for the population as a whole. The truth is, obesity isn’t simply about overeating or laziness. It’s a chronic disease, and treating it like one is the only way forward.
When we call something a chronic disease—like high blood pressure, diabetes, or asthma—it means it’s long-term, it’s manageable but not always curable, and it requires consistent attention. Obesity fits this definition. It doesn’t go away with a 30-day cleanse. It doesn’t disappear after a few weeks at the gym. And it’s not just about the number on the scale. It’s about what excess weight is doing to your joints, your organs, your sleep, your energy, and your overall health.
Why Treat It as a Disease?
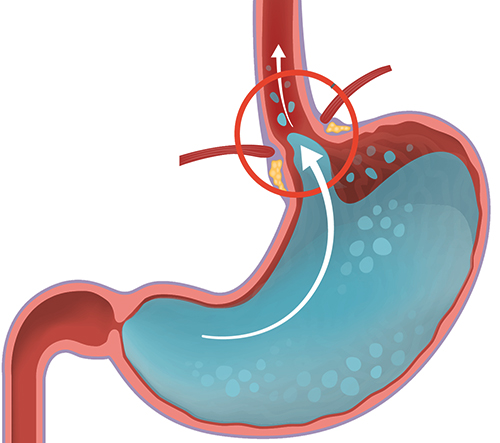
First, let’s be clear: obesity changes how your body works. Hormones that regulate hunger, metabolism, and fat storage get out of balance. Insulin becomes less effective, blood sugar rises, and inflammation becomes a constant presence. These are real, measurable biological changes—not excuses. And they’re hard to undo with simple lifestyle tweaks alone.
Treating obesity as a chronic disease shifts the goal from short-term weight loss to long-term health management. It also removes the shame and finger-pointing that have plagued the conversation for decades. You wouldn’t blame someone for needing medication to control blood pressure. So why shame someone who needs support to manage their weight?
What Real Management Looks Like
Managing obesity starts with understanding your baseline. That includes more than just weight. It’s about waist size, blood sugar, cholesterol, blood pressure, liver function, and mobility. These markers help define the risks and guide the approach.
Next comes a sustainable plan—not a crash diet. This often includes:
-
Food that supports your goals, not punishes you: More protein, fiber, and healthy fats. Fewer processed carbs and sugary drinks. Regular meals to avoid binge cycles.
-
Movement that fits your body: This might mean walking, stretching, swimming, or light strength training. The point isn’t to suffer—it’s to build momentum and protect your joints and muscles.
-
Sleep and stress control: Poor sleep and chronic stress raise hormones that increase appetite and fat storage. Fixing these isn’t about bubble baths and meditation apps—it’s about practical things like turning off screens earlier, avoiding late caffeine, and dealing with daily problems in manageable ways.
-
Medical options: For many, especially those with severe obesity or related conditions, medications or surgery are part of the plan. This isn’t giving up. It’s using the tools available. New medications like GLP-1 receptor agonists (such as semaglutide) are changing the game—not as magic bullets, but as aids to level the playing field.
Consistency Beats Perfection
Managing obesity isn’t about perfection. Some days are better than others. The trick is not letting one bad day become a bad week, or a bad year. Like any chronic condition, it’s about adjusting as life changes—keeping regular appointments, watching trends, and staying ahead of problems before they spiral.
That also means preparing for plateaus. At some point, weight loss may stall. That doesn’t mean failure. The body defends its fat stores more fiercely than most people realize. When progress slows, it’s a sign to reassess—not to quit. What’s working? What’s changed? What needs tweaking?
Avoid the Quick Fix Trap
There’s always a new fad: a miracle food, a brutal detox, a “one weird trick” video. These are distractions. They might offer fast results, but they rarely last. The best strategy is usually the most boring: real food, regular movement, honest tracking, and support.
The diet industry thrives on quick fixes that don’t work long-term. The healthcare approach should do the opposite: create steady, realistic, personalized paths that people can follow for life—not just until swimsuit season.
Support That Matters
Obesity isn’t solved in isolation. Having a doctor who listens, family who helps, and a system that supports—not shames—can make a huge difference. Support doesn’t mean being soft. It means being smart and steady. It’s about practical adjustments, not pep talks.
Employers, schools, and communities can also step up. Affordable healthy food, safe places to walk, and reasonable work hours help more than judgment ever will.
Final Thoughts
Obesity is complex. It’s influenced by biology, environment, culture, and habits. But it’s not hopeless. When treated like the chronic condition it is—with consistent care, smart choices, and the right tools—people can live healthier, stronger, longer lives.
This isn’t about chasing skinny. It’s about chasing strength, energy, and control over your body. That’s not a slogan. It’s a strategy. And it works.