In the quiet hours of the evening, when the day slows down and the body finally rests, many people are met not with peace—but with a burn rising through their chest. Heartburn, an uninvited guest, has become an all-too-familiar discomfort in today’s world. What’s less widely discussed, however, is its complex and insidious link with another modern-day epidemic: obesity.
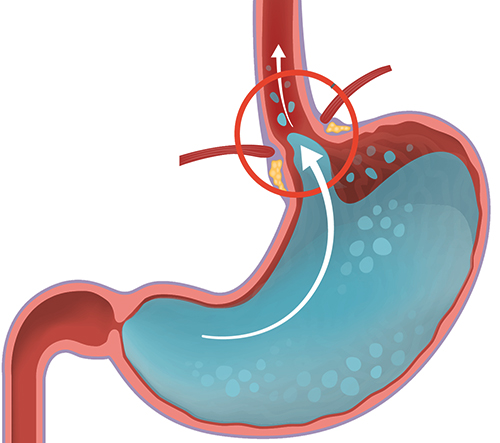
The relationship between obesity and heartburn isn’t just coincidental—it’s deeply physiological. As waistlines expand, so too does the pressure inside the abdomen. This pressure doesn’t just stay put; it pushes upward, against the stomach, squeezing its contents toward the esophagus. The result is gastroesophageal reflux—acidic stomach contents creeping past the lower esophageal sphincter, a valve meant to keep the stomach’s contents in their rightful place.
For those who carry extra weight—particularly around the midsection—the mechanical strain on the digestive system is persistent. Even lying down or bending over can become triggers. And so, meals that should bring satisfaction instead bring discomfort, sour tastes, and sleepless nights.
But it’s not just about pressure and mechanics. Obesity also alters the body’s chemistry. Fat tissue, particularly visceral fat around the organs, is metabolically active. It releases inflammatory compounds and hormones that can disrupt normal digestive function, weaken the esophageal sphincter, and make heartburn more frequent and severe. In this way, obesity doesn’t just nudge the door open for acid reflux—it helps it settle in.
For many, heartburn is written off as a minor nuisance—an occasional price to pay for a spicy meal or a late-night snack. But chronic acid reflux, medically termed gastroesophageal reflux disease (GERD), can lead to long-term damage. The esophagus isn’t built to withstand the corrosive touch of stomach acid. Over time, this can result in inflammation, ulcers, and even precancerous changes in the esophageal lining.
This growing intersection between obesity and heartburn is mirrored in global trends. As rates of overweight and obesity climb worldwide, so too does the prevalence of GERD. In many countries, the two now go hand in hand, a reflection of broader lifestyle shifts: more processed food, less physical activity, more sedentary hours.
Yet this narrative doesn’t have to be a closed loop. Even modest weight loss can have a significant impact. Studies show that losing just 10% of body weight can reduce the severity and frequency of reflux symptoms. It’s a reminder that small steps—like mindful eating, regular movement, and managing meal timing—can shift the story.
In the end, the link between obesity and heartburn isn’t just a tale of biology—it’s a reflection of how our bodies respond to the environments we create. It’s a quiet, persistent conversation happening within, reminding us that health is not just about how we look, but how we feel—and how we live.